The Military Health System and Substance Abuse Coverage for Veterans
TRICARE Insurance covers military departments such as the U.S. Air Force, Marine Corps, and other major branches of our armed services. With the current wave of veterans suffering from drug and alcohol use disorders, finding efficient supplementary insurance that offers substance abuse treatment coverage and mental health services.
In this article, we’ll review TRICARE Insurance and answer questions, such as ‘Does TRICARE cover alcohol rehab?’ and much more. If you’re a current or former service member suffering from issues with alcohol, it is estimated that around 1 out of every 10 current and former members of the military suffer from a major substance abuse issue. These substance abuse issues range anywhere from individual drug and alcohol problems to dual diagnosis challenges and more.
Without proper coverage for things like medically supervised detox, residential treatment, outpatient treatment, and other levels of care, finding a solution for such substance abuse challenges is nearly impossible. You and your loved ones may already know how difficult the struggle to get help can be, but help is here.
Keep reading our blog to get details on TRICARE coverage for addiction treatment, and how South Shores Detox and Recovery tailor our programs to help veterans find lasting recovery!
What Is a Supplementary Insurance Plan?
In some cases, a service member may have difficulties obtaining approval for full coverage in regard to certain forms of substance abuse treatment. This includes things like medication assisted treatment, prescriptions involved with detox and withdrawals, and more.
In these cases, organizations like TRICARE Insurance can provide what’s known as supplementary coverage. This can cover additional costs that standard health insurance might not pay for in full – such as drug rehab and attached services like intensive outpatient programs and more.
But what does TRICARE Insurance cover exactly, and how can it benefit you?
A Brief Background on TRICARE Health Insurance
TRICARE Health Insurance, as mentioned above, was previously known by a different name. These changes took place around 2017, and the name wasn’t the only overhaul the company experienced.
TRICARE coverage also expanded its offerings to include more comprehensive options for drug and alcohol addiction. Whether this was directly influenced by the recognition of the growing problem of veterans requiring substance abuse treatment remains a mystery.
However, after the Affordable Cares Act, most providers were forced to begin providing coverage for drug and alcohol treatment at some level.
What Alcohol Treatment Programs are Covered by TRICARE?
Several different TRICARE plans exist, and ultimately your specific coverage determines what services and how much is covered. However, as a rule, you can expect to receive at least some type of coverage for the following:
- Intensive Outpatient Programs
- Partial Hospitalization Programs
- Residential Treatment
- Treatment Services Involving Family Members
- Mental Health Treatment Programs
- and several other addiction treatment programs
Does TRICARE Cover Alcohol Detox Services?
Detoxification is the initial step in the journey of many clients to sobriety, and it involves the medically supervised and monitored elimination of the abused substance from the body. Because of the intense discomfort of withdrawal, detox is a challenging process.
Cold chills, exhaustion, painful muscle tension, heart palpitations, irregular heartbeat, and seizures are all possible physical symptoms of this condition. Becoming fully sober after long-term substance abuse is a necessary first step toward recovery from addiction, and medical detox is a crucial part of that process.
South Shores Detox’s medical detox program is staffed around the clock since we understand how challenging the withdrawal process can be. Our clients may spend anywhere from a few days to a few weeks in detox, depending on the severity of their addiction.
Detoxification is only covered by your TRICARE plan if it is received in a hospital setting, regardless of how long it takes you to finish the process. This falls under the emergency or hospital designation, which is covered further in the section below.
Does TRICARE Cover Residential Treatment?
Several important situations must take place in order for TRICARE to provide coverage for inpatient treatment services. The client must have an official diagnosis, experience intense withdrawal, and suffer from a significant decline in quality of life because of their drug addiction.
If these conditions are met, TRICARE will pay for inpatient addiction treatment, whether it’s through admittance via emergency or a formal drug rehab intake. When a client has a mental or physical crisis that necessitates quick medical attention, this falls under the guise of emergency care – a designation nearly always covered by TRICARE.
It is worth noting that the military will know about rehab attendance more certainly if using this form of insurance, and keeping confidential is more difficult than with private pay or other forms of insurance.
Does TRICARE Cover Alcohol Rehab: The Full Spectrum of Coverage
Detoxification, stabilization, and maintenance are also covered by TRICARE. When an individual agrees to enter treatment for substance misuse on their own, this is known as non-emergency care. Before TRICARE will pay for this, the parameters mentioned above must be met. Detox and stabilization services are typically covered, and depending on the policy, additional mental health disorder therapy may also be covered as part of addiction treatment.
In some cases, addiction treatment coverage requires prior authorization from a primary care doctor or professional at the mental health facility. At South Shores Detox and Recovery, these authorizations are commonly provided on short notice to get our clients’ fast approval and admittance into our program.
TRICARE and Outpatient Substance Abuse Programs
Many service members, past and present, may be curious about outpatient addiction treatment. TRICARE provides coverage for this level of care, assuming certain requirements are met.
For a client to receive approval for outpatient coverage, they must receive a diagnosis for their substance abuse disorder but NOT require 24/7 monitoring or emergency medical care. Generally, outpatient services fall under one of three separate designations:
- Standard Outpatient
These standard treatment services are the most basic form of substance abuse treatment. Generally, a client participates in therapy sessions (individual and group) at the facility for 2-4 hours weekly, twice per week.
The therapy prescribed at this level of care is identical to the mechanisms used for inpatient. However, the efforts are usually far less intensive, with certain offerings not included like additional or supplementary forms of therapy (art, equine, etc.)
- Intensive Outpatient
Intensive outpatient is offered as an alternative to standard outpatient addiction treatment services. This treatment is mostly used as a step down from inpatient drug rehab services and standard outpatient addiction treatment services.
Alternatively, intensive outpatient may also be prescribed in events where clients attempted the standard form of this recovery plan and faltered along the way. However, it’s most commonly used in some form similar to the situation mentioned above, as an aftercare component to residential treatment.
- Partial Hospitalization Programs
PHP programs are most like inpatient care regarding the intensity of treatment and modalities of therapy. These are generally reserved for more severe cases of a substance use disorder, but for clients, who for some reason or another, can’t fully participate in a residential program.
Clients who must maintain some form of job or remain at home daily for family purposes or otherwise are generally prime candidates for PHP. Alternatively, some clients may opt for PHP as a segue between inpatient and outpatient recovery programs.
This is often recommended by many doctors if a client has the option, as taking smaller, more micro-managed steps back into regular society often produces higher rates of success in regard to long-term recovery efforts.
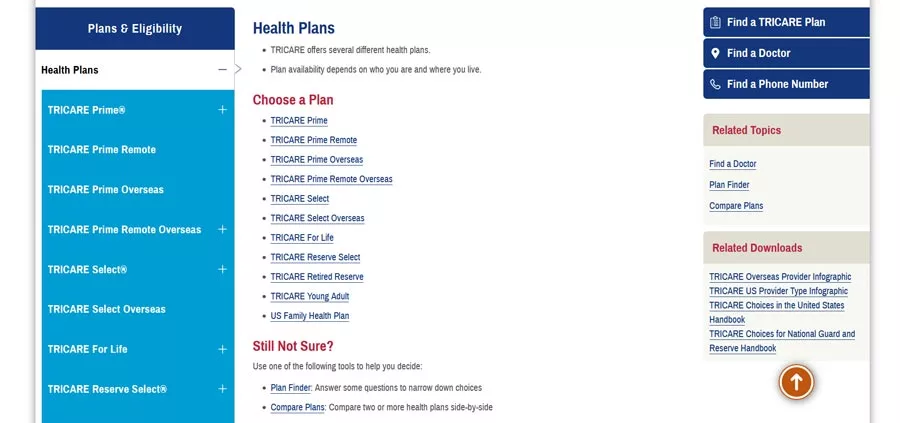
What are the TRICARE Plan Options?
TRICARE Prime
This plan is for active duty and retired members of the military, including active and retired reserves and the families of all of the previously mentioned groups. However, retired members who may receive Medicare are not eligible for Prime.
Other TRICARE Prime Options include:
- TRICARE Prime Remote.
- TRICARE Prime Overseas.
- TRICARE Prime Remote Overseas.
- TRICARE Select
TRICARE Select
TRICARE Select is a PPO (preferred provider) plan. If you’re on active duty, full time or reserves, you are not eligible for TRICARE Select. Ideal candidates for TRICARE Select include:
- Those with employee sponsored insurance
- See a treatment provider outside of the regular network
- Live in an area where TRICARE Prime is not an option
TRICARE for Life
TRICARE for Life is reserved for those who have Medicare Part and B, with no reservations regarding age or geographic location. Enrollment is not required, and coverage is automatic for all eligible. To receive these benefits, one must produce a military ID at the offices of any doctor or physician across the globe.
TRICARE Reserve Select
This premium plan is available anywhere for reserve members and their immediate families.
However, you are ineligible if:
- You’re on active duty or deployed
- Eligible for Federal Health Benefits
- Covered under the Transitional Assistance Management Program
TRICARE Retired Reserve
This premium option is solely for those who are retired reserve members UNDER the age of 60. You must not be eligible for Federal Employees Health Benefits.
TRICARE Young Adult
This plan is reserved for adult children who are not eligible for TRICARE coverage. You must be an adult child or dependent of an eligible recipient of TRICARE and single and over the age of 21 but no older than 26.
South Shores Works with TRICARE to Promote Your Sobriety
South Shores Detox and Recovery is an in-network partner of TRICARE Insurance. This means your out-of-pocket costs are minimal compared to out-of-network options, and we have an ongoing relationship with the TRICARE organization that allows us to create a seamless admissions and billing process.
The last thing you need is stress over financials when you’re attempting to recover. For more peace of mind and focus on your well-being, contact a member of our staff regarding admissions and put your insurance to work today!